Fixing Health Inequities and Access to Care : This TrenBuzz feature explains — step by step — why health inequities and uneven access to care remain among America’s most urgent problems in October 2025, how they show up in real communities (maternal health deserts, mental-health black spots, rural hospital closures), what the latest data and policy landscape say, and practical, high-impact actions readers can take right now. All claims below are drawn from official and peer-reviewed reporting; verified links are at the end.
Fixing Health Inequities and Access to Care: Why this matters (one short paragraph)
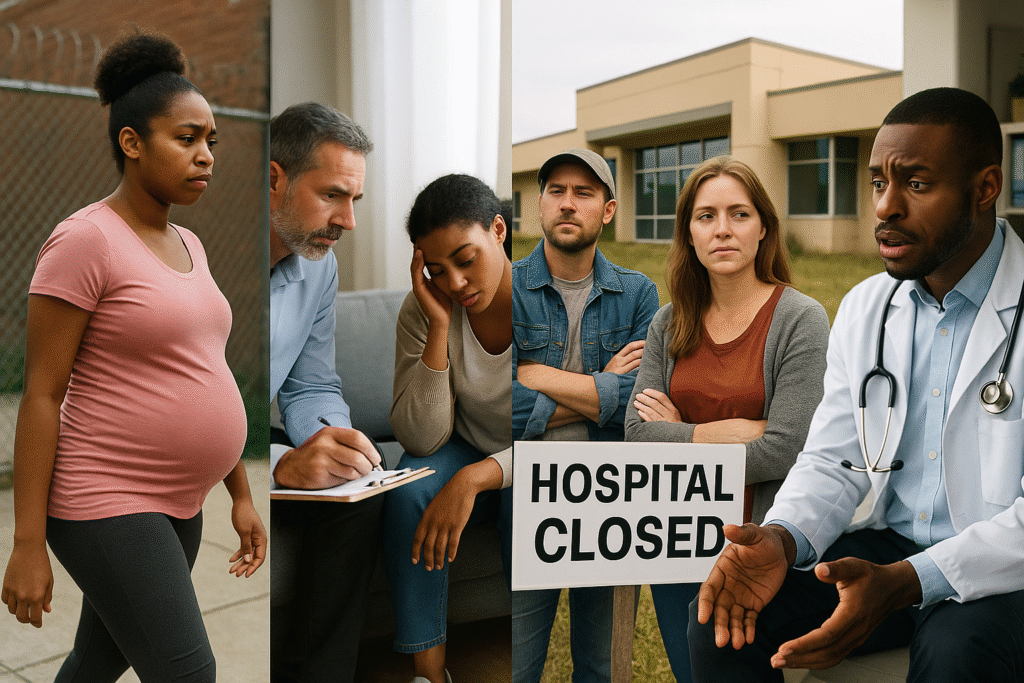
Health inequities mean that where you are born, the color of your skin, your income and whether you live in a city or on a rural county road still predict how long you will live, whether you will get timely prenatal care, and whether a clinic is available when you’re sick. Fixing these gaps improves lives and lowers health costs — but it requires targeted policy fixes, sustained funding, and local action.
1) What the data shows right now (the big signals)
• Racial and ethnic disparities persist across maternal mortality, chronic disease outcomes, vaccination uptake and COVID/long-COVID harms. National trackers and the Commonwealth Fund document persistent gaps in coverage and outcomes across groups.
• Geographic disparities are severe: many counties — especially rural and tribal areas — lack obstetric services (“maternity care deserts”), behavioral-health clinicians or an open hospital within reasonable driving distance. Research and public-health reviews connecting maternal-care deserts to higher pregnancy complications have appeared in peer-reviewed journals in 2025.
• Insurance & policy gaps: Medicaid expansion has materially narrowed access gaps where adopted — but as of Oct 2025 ten states still have not expanded Medicaid, leaving coverage holes for low-income adults. KFF’s state tracker and NCSL maps remain the best sources for who has expanded and who has not.
• Rural hospital closures: From 2017–2024 dozens of rural hospitals closed and many more operate on thin margins, shrinking local inpatient capacity and emergency access. KFF and UNC Sheps Center data document this pattern and its consequences for local care access.
Those four trends — race, place, policy and facility availability — combine to make a patchwork U.S. system where national averages hide local crisis points.
2) How inequities show up in everyday life (concrete examples)
- Pregnancy and childbirth: Some counties have zero obstetric providers. In those maternity-care deserts, pregnant people travel far for prenatal visits or deliver far from home — raising the odds of delayed care and severe complications. The Commonwealth Fund and maternal-health reviews highlight these relationships.
- Behavioral health: School counselors, child-psychiatry slots and adult therapists are concentrated in urban centers. State reports and the 2025 State of Mental Health in America snapshot show many states with high youth mental-health needs but poor access to care. Medicaid is a major payer for behavioral health — so states that have not expanded Medicaid leave many adults uninsured.
- Rural emergencies: When a rural hospital closes, ambulance trips get longer, transfers increase, and time-sensitive care (stroke, sepsis, trauma) is harder to access. KFF’s rural hospital briefs show dozens of closures and many slender margins across the sector.
- Preventive services & sexual health: In states with clinic closures (including recent Planned Parenthood clinics), gaps in contraception, STI screening and cervical-cancer prevention are immediate and measurable — with long reach into maternal and reproductive health outcomes.
These are not abstract patterns — they shape real choices (whether to drive 2 hours for prenatal care), real harms (missed vaccinations, untreated depression), and real costs (higher emergency visits, worse birth outcomes).
3) The policy levers that actually move the needle
Below are evidence-backed policy actions shown to improve access and reduce inequities. Each one is actionable at state or federal level.
- Medicaid expansion — Where states expanded Medicaid under the ACA, low-income adults gained coverage and access to mental-health and primary care. Closing the 10-state gap would yield large immediate coverage gains. KFF documents the state-by-state differences and the evidence that expansion improves access.
- Invest in health centers & community clinics — HRSA-funded community health centers served a record 32+ million patients in 2024 and are proven anchors for underserved communities, providing primary care, prenatal services and behavioral health integration. Bolstering these centers with sustained funding expands reach fast.
- Support rural hospitals & rural health funds — The 2025 reconciliation law included a $50 billion rural health fund designed to stabilize rural providers — how funds are allocated matters, but dedicated rural support helps keep local inpatient capacity and emergency care. KFF explains the fund and the implementation choices states face.
- Grow the behavioral-health workforce — Loan repayment, targeted residency slots for psychiatry and incentives for community-based providers close gaps quickly. State policies that create school-based mental-health teams also help youth access care. KFF and APHA outline concrete workforce strategies.
- Targeted maternal-health investments — MMRC-driven reforms, doula and midwifery integration, and support for rural birthing centers reduce maternal mortality in high-risk counties. Commonwealth Fund and academic reviews map successful state interventions.
These levers are proven or strongly evidence-informed — they work best when combined, not used in isolation.
4) Short-term, high-impact actions communities and readers can take now
You don’t need to be a lawmaker to make a difference. Here’s a ready-to-use playbook, from quick wins to deeper engagement:
- Call or email your state legislators about Medicaid expansion (if your state hasn’t expanded). Use the script below. KFF’s tracker shows which states remain on the fence.
- Volunteer or donate to your local health center — HRSA’s health center finder points you to nearby clinics that welcome volunteers and unrestricted donations to support sliding-scale care.
- Support maternal-health programs: local doulas, postpartum support groups and transportation programs reduce birthing risks. Community foundations often run matching funds. Commonwealth Fund briefs list model programs for state replication.
- Promote behavioral-health access in schools: petition your school board to fund on-site counselors or tele-psychiatry for students; evidence shows school-based services increase access and reduce emergency room use.
- Back rural hospital stabilization: contact county officials urging transparent use of rural health funds and support for local hospital operating grants. KFF and state briefs explain funding options.
Small actions add up: a few volunteers per clinic per week, one phone call to a lawmaker, or a modest donation to a community doula program can change individual lives.
5) What a practical advocacy script sounds like
Use this 30-second template when you call or email:
“Hi — I’m [Name] from [Town, ZIP]. I’m concerned about access to care in our community. Please support (1) Medicaid expansion in our state so more low-income residents get covered, (2) increased funding for community health centers and (3) a dedicated plan to keep rural hospitals open. These steps will improve maternal care and behavioral-health access where it’s needed most. Will you support these policies?”
If you want a ready-to-send email or social tile, I can create one for your TrenBuzz readers.
6) How journalists and local editors should cover this (editor’s checklist)
- Localize the data. National headlines miss the county-by-county reality; embed county maps and HRSA/CDC local indicators.
- Tell human stories ethically. Profile a new mom in a maternity-care desert or a school counselor managing 200 students — real people make policy stakes clear.
- Verify funding claims. When a state says it’s “protecting rural hospitals,” ask for budget line items and implementation timelines. KFF and state budget trackers are essential.
- Provide actions. Every story should end with 2–3 concrete steps readers can take (volunteer links, advocacy scripts, donation options). Readers appreciate practical next steps.
This approach increases trust, drives constructive engagement, and helps communities get results.
7) Common questions (short Q&A)
Q: Will Medicaid expansion alone fix access problems?
A: No — expansion is one big lever that increases coverage and access, but clinics, workforce and hospital capacity still need investment. Combine expansion with clinic funding and workforce programs for real results.
Q: Are rural hospital closures inevitable?
A: Not inevitable. Targeted funding (rural health fund), flexible Medicare payment models and state stabilization grants can keep facilities open. The 2025 rural fund is designed to help, but allocation matters.
Q: How quickly can maternal mortality improve?
A: Improvements are possible within a few years when states invest in perinatal systems (MMRC recommendations, improved transfer networks, expanded midwifery/doula programs). But sustained attention is required.
8) The role of philanthropy and private sector (how they can help today)
Private dollars can jump-start programs: fund rural telehealth hubs, sponsor school-based mental-health positions, and subsidize transportation for prenatal care. Corporate Medicaid managed-care partnerships can extend community outreach — but they work best when paired with public funding and local oversight. Models from states that blended philanthropic pilots with public matching show scalable successes.
9) Measuring success — quick metrics for local progress
If you run a clinic or are tracking a campaign, use these short indicators:
- % uninsured in county (pre/post policy change) — KFF tracks state/county coverage.
- Number of active OB/GYN or CNM providers per 10,000 births (maternal access metric).
- School counselors per 1,000 students and wait time for youth behavioral-health appointments.
- Emergency transfer times and distance to nearest open hospital (rural access metric).
These metrics let local leaders show fast wins and justify further investment.
10) Final takeaway — the short version for busy readers
Health inequities and access gaps are solvable problems if states and communities combine policy (Medicaid expansion, rural-fund investments), clinic funding (HRSA health centers), workforce programs (loan repayment, training pipelines) and targeted maternal and behavioral-health support. Small local actions — volunteering, calling state reps, donating to a clinic — add up and push policy change. The time to act is now.
Verified external links
(Only the primary, reputable sources used in this article are listed below. Click any item to read the original reporting or data.)
- KFF — Status of State Medicaid Expansion Decisions. (KFF)
https://www.kff.org/medicaid/status-of-state-medicaid-expansion-decisions/ - HRSA — About the Health Center Program / Impact (32.4M patients in 2024). (bphc.hrsa.gov)
https://bphc.hrsa.gov/about-health-center-program - Commonwealth Fund — State of Maternal Health 2025 & health-disparities resources. (Commonwealth Fund)
https://www.commonwealthfund.org/publications/issue-briefs/2025/jul/maternal-mortality-united-states-2025
https://www.commonwealthfund.org/health-disparities - KFF — 10 Things to Know About Rural Hospitals (closures and trends). (KFF)
https://www.kff.org/health-costs/10-things-to-know-about-rural-hospitals/ - State of Mental Health in America 2025 (Mental Health America report). (Mental Health America)
https://mhanational.org/stateofmentalhealth2025 - Peer-reviewed article on maternal-care deserts (2025). (PMC)
https://pmc.ncbi.nlm.nih.gov/articles/PMC12258799/ - Trust for America’s Health — Public Health Infrastructure and workforce analyses (2025). (PMC)
https://www.tfah.org/report-details/funding-report-2025/ - AP News — Planned Parenthood clinic closures in Louisiana: local access impacts (Oct 2025). (AP News)
https://apnews.com/article/planned-parenthood-louisiana-clinics-close-2025 - KFF brief — $50 Billion Rural Health Fund (2025 reconciliation law explainer). (KFF)
https://www.kff.org/medicaid/a-closer-look-at-the-50-billion-rural-health-fund-in-the-new-reconciliation-law/
Disclaimer
This article is editorial and synthesizes public reports and peer-reviewed research as of October 2025. It is not medical or legal advice. For individual clinical questions, consult your healthcare provider. For official policy documents, consult primary sources listed above (HRSA, KFF, Commonwealth Fund) and state health departments for localized details. Images used in this article are royalty‑free or licensed for commercial use and are provided here for illustrative purposes.